| date | description |
|---|---|
| 2025-07-04 | MRI Scan (Magnetic Resonance Imaging) |
| 2025-06-25 | FOLFIRI + aflibercept fourth chemotherapy session (tenth chemo round) |
| 2025-06-11 | FOLFIRI third chemotherapy session (ninth chemo round) |
| 2025-05-28 | FOLFIRI second chemotherapy session (eigth chemo round) |
| 2025-05-23 | First radiotherapy session to treat tumor masses on my hip (1/5) |
| 2025-05-20 | Simulation TAC andy radiologist appointment to treat the leg problem |
| 2025-05-14 | FOLFIRI first chemotherapy session (seventh chemo round) |
| 2025-05-07 | Latest CT scan confirms that FOLFOX is not effective, so the decision has been made to switch to FOLFIRI. They can't administer it today because my immune defenses are too low. |
| 2025-04-29 | Radiotherapy session to treat tumor masses on my shoulder and biceps |
| 2025-04-28 | TAC to check there's no oclussion |
| 2025-04-28 | Visit to the emergency room due to lack of bowel movements and abdominal pain |
| 2025-04-23 | Sixth chemoteraphy session FOLFOX+veba |
| 2025-04-16 | Radiotherapy session to treat tumor masses on my back (5) |
| 2025-04-15 | Radiotherapy session to treat tumor masses on my back (4) |
| 2025-04-14 | TAC de control |
| 2025-04-14 | Radiotherapy session to treat tumor masses on my back (3) |
| 2025-04-12 | Radiotherapy session to treat tumor masses on my back (2) |
| 2025-04-11 | Radiotherapy session to treat tumor masses on my back (1) |
| 2025-04-09 | Fifth chemoteraphy session FOLFOX+veba |
| 2025-04-08 | MRI Scan (Magnetic Resonance Imaging) |
| 2025-03-29 | Emergency room visit due to high fever and back pain |
| 2025-03-27 | Fourth chemoteraphy session FOLFOX+veba |
| 2025-03-25 | Emergency room visit due back pain |
| 2025-03-12 | Third chemoteraphy session |
| 2025-03-07 | Blood test to monitor trasaminases. Still going down a bit, stabilizing. |
| 2025-03-04 | 38-degree fever in the afternoon. I take Paracetamol at 7 PM. Around 9:30 PM, starts to go down and finally disappears. |
| 2025-03-04 | I resume Atocet as values return to normal. |
| 2025-03-04 | Blood test to monitor trasaminases. Starts to go down. |
| 2025-03-03 | Drop Azotet due high trasaminases values |
| 2025-03-01 | Blood test to monitor trasaminases. Still rising. |
| 2025-03-01 | Brain radiotherapy session (5) |
| 2025-02-28 | Brain radiotherapy session (4) |
| 2025-02-27 | Medication: Jardiance Reduce blood sugar. Good Chemotherapy synergies |
| 2025-02-27 | Medication: Hidroferol Vitamin D. Good Chemotherapy synergies |
| 2025-02-27 | Brain radiotherapy session (3) |
| 2025-02-26 | Start of the second round of chemotherapy |
| 2025-02-26 | Medication: Azotet Reduce cholesterol. Good Chemotherapy synergies |
| 2025-02-26 | Brain radiotherapy session (2) |
| 2025-02-25 | Brain radiotherapy session (1) |
| 2025-02-10 | Start of the first round of chemotherapy FOLFOX treatment |
| 2025-01-31 | Hospital admission due to intestinal obstruction (hospitalized until February 13) |

(02-25-2025) I’m starting brain radiotherapy to treat the brain metastases.
(04-11-2025) I’m starting radiotherapy to treat the tumor masses on my back.
(04-16-2025)) Today I finished the 5 radiotherapy sessions for the mass on my back. I’d like to think that the sharper pain has eased. It still hurts, but that’s the feeling I get. It could also be because I’ve barely moved from bed these past three days due to fatigue. We’ll see how it evolves. Also, before the last session they did a new CT scan (for radiotherapy), in order to properly locate the ones on the shoulder and biceps. They’ll let the body rest for a week, and the plan is to target those two lumps next.
(04-29-2025) Radiotherapy session targeting left shoulder and biceps.
(05-09-2025) Second radiotherapy session targeting left shoulder and biceps.
At first, I had no symptoms. However, as I was warned, the areas where the lesions were "targeted" may lose hair.
(15-03-2025) Unfortunately, 15 days later, that’s exactly what happened. My hair has started falling out in some areas. Even though it may seem trivial, for me, this is a tough psychological blow.
(17-03-2025) I decide to shave my head 😭
(16-04-2025) It’s possible that part of the fatigue I’m feeling is due to the radiotherapy.

(08-04-2025) Brain MRI scan. This test was moved up by a few weeks, so the results should possibly be better. Nevertheless, it was detected that the brain radiotherapy sessions I underwent between February 25 and March 1 are working.
Below is a comparison of the size of the metastatic lesions compared to those on February 4.
| Area | 04/02/2025 | 08/04/2025 | % change |
|---|---|---|---|
| Right cerebellar hemisphere | 0.7 cm | 0.4 cm | -42.9% |
| Right cerebellar hemisphere | 2.4 cm | 2.1 cm | -12.5% |
| Right temporo-occipital | 1.9 cm | 1.3 cm | -31.6% |
| Right frontal operculum | 0.8 cm | 0.5 cm | -37.5% |
| Left frontal | 1.7 cm | 1.4 cm | -17.6% |
| Left frontal | 1 cm | 0.5 cm | -50% |
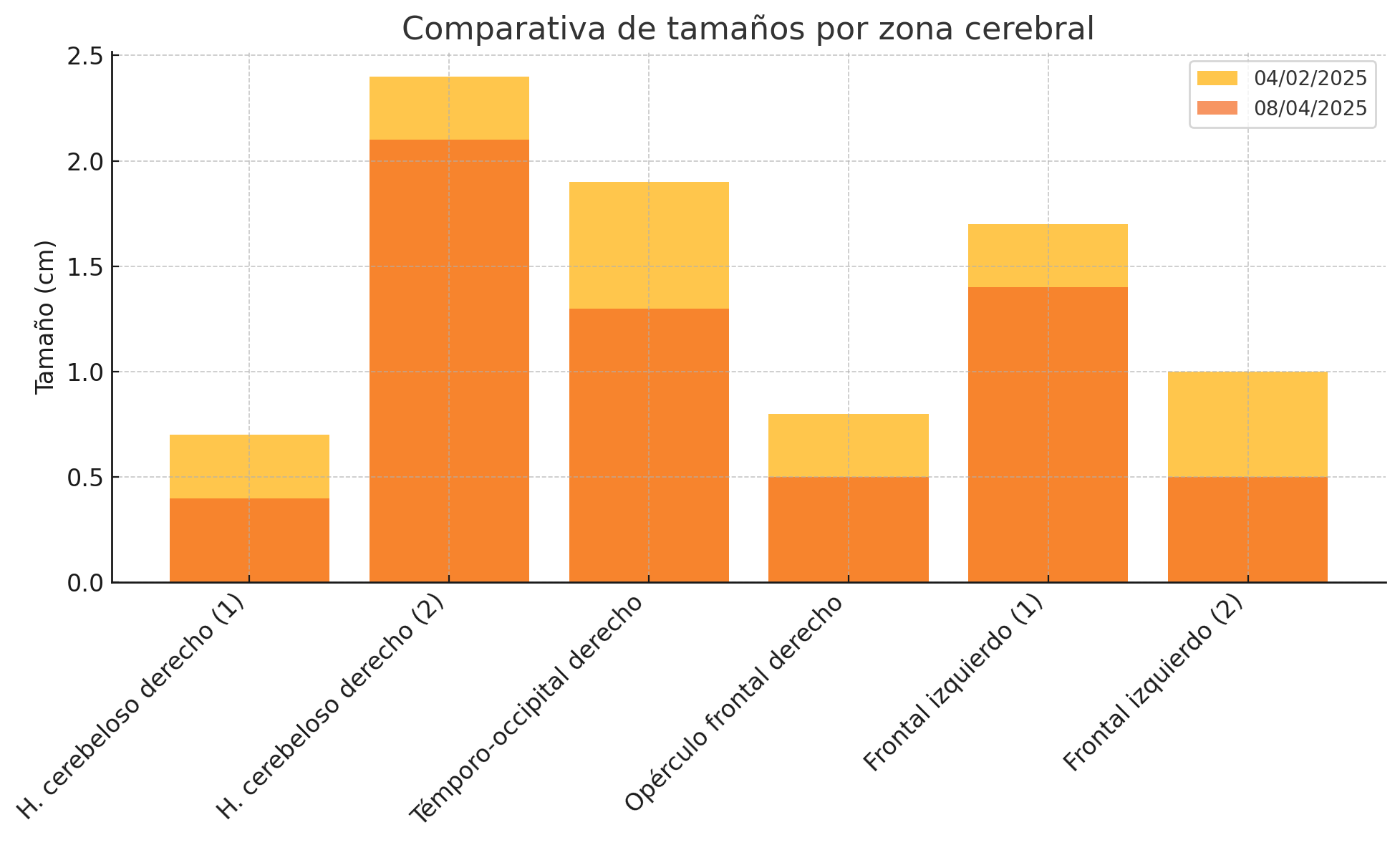
In total, a 27.1% reduction.

Blood test were even better this time.
I spent the whole session sleeping, so it felt not so long this time.
Next session in 15 days.
(23-06-2025) We went to the emergency room because of a very intense pain in the middle of the intestine. It seems it’s nothing serious and we’re treating it with Nolotil. I started this session at 63 kg and it looks like I’m finishing it at 59 kg. I’ve completely lost my appetite.
Blood tests came back fine. So they administered the dose as usual.
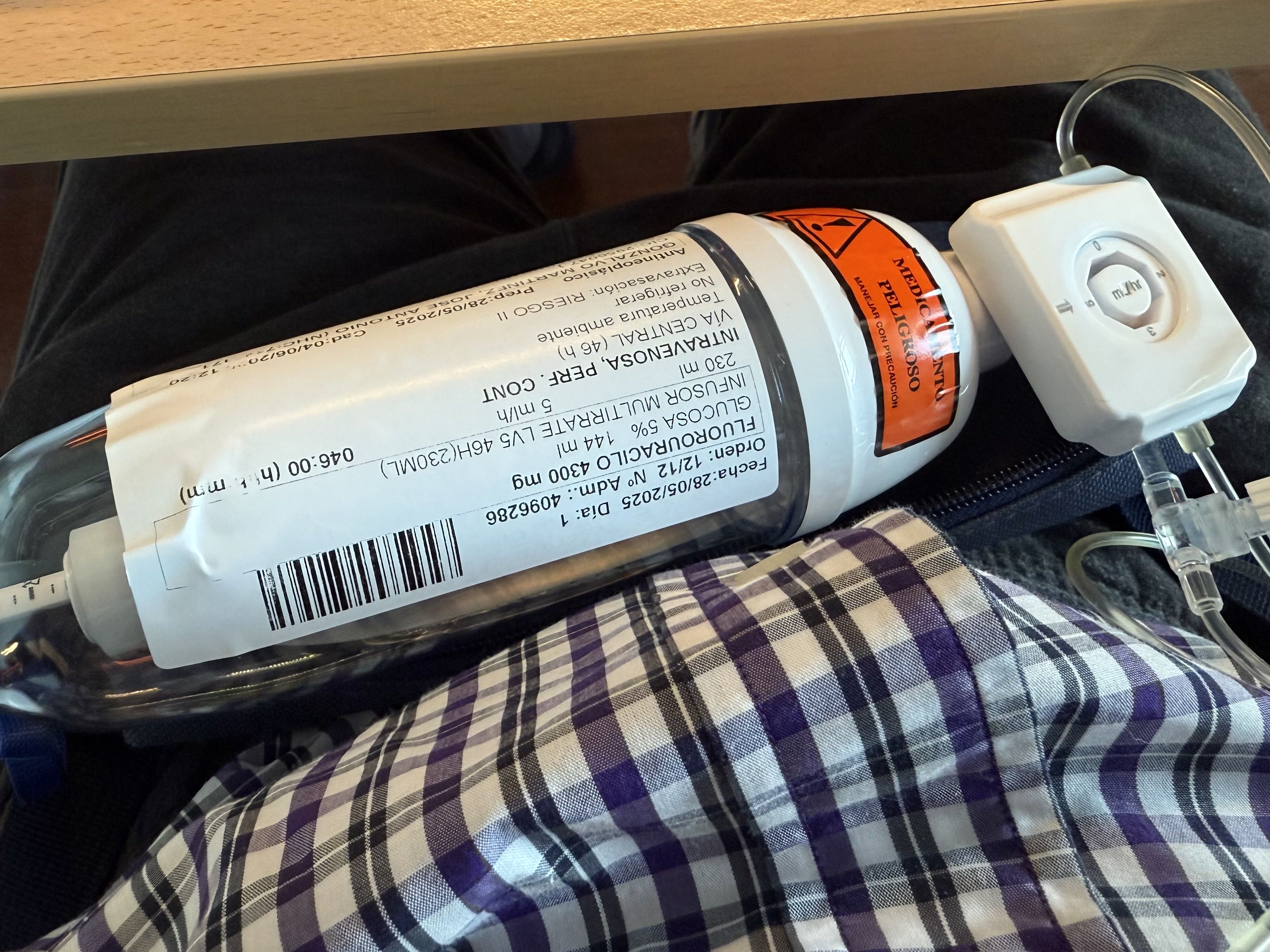
Out of curiosity, here’s a photo of all the “poisons” they inject me with in one session:

In addition to this, there’s the cherry on top, which is the infuser that I stay connected to for 2 more days.
Next session in 15 days.
Blood test results are quite good, although I’m starting to develop anemia. So, before starting the chemotherapy session, they give me an iron IV.
We are changing the chemo regimen from FOLFOX to FOLFIRI.
The most significant expected side effect is diarrhea.
Next session in 15 days.
As usual, the day started with a blood test to see whether it was possible to go ahead with the chemo round.
Later, there was an appointment with the oncologist, who reviewed the test results and gave the go-ahead for the chemotherapy. All good again. Defenses are a bit low, but it seems that’s normal.
Theoretically, today the oncologist was supposed to give us the results of the follow-up CT scan and her assessment. However, the CT report was still not available (!?) — 9 days later. So we left without knowing how things are going. The report has been urgently requested, but the oncologist’s assessment will now have to wait until the next chemo round on May 7th.
After a few hours of waiting, I went into the room where they administer the chemotherapy. Once that was done, they hooked me up to the infuser, which delivers the final dose of chemo over the next couple of days. I’ll go in on Friday afternoon to have it removed.
On the way home, we were able to access the CT scan report online.

Full day. First thing in the morning, routine blood tests. These tests are always done before a round of chemo to make sure the body is going to be able to handle it.
Then, an appointment with the radiologist to review the brain MRI from the day before. The results are positive and, more or less, as expected at this stage.
They also considered applying radiotherapy to the tumor masses I have on my back, shoulder, biceps... especially the one on my back, which has me completely incapacitated. In the end, they did a simulation CT scan and, theoretically, I’ll receive five sessions starting Friday, with the goal of reducing the size of those masses and relieving the pain.
After that, I moved on to the check-up with the oncologist on duty. After reviewing my case and current condition, I was cleared to receive the session.
At 1:30 PM I started chemo and we finished around 7:30 PM.
Next session in two weeks, on April 23.

This time they’ve added Bevacizumab, which complements FOLFOX and enhances its effects—for better or worse. It has several side effects, such as bleeding, high blood pressure, and increased strain on the liver.
Due to the back pain, I’ve gone back to Dexamethasone (corticosteroids). The upside is that they’re moving up my CT scan and/or a IMR Scan to early April.
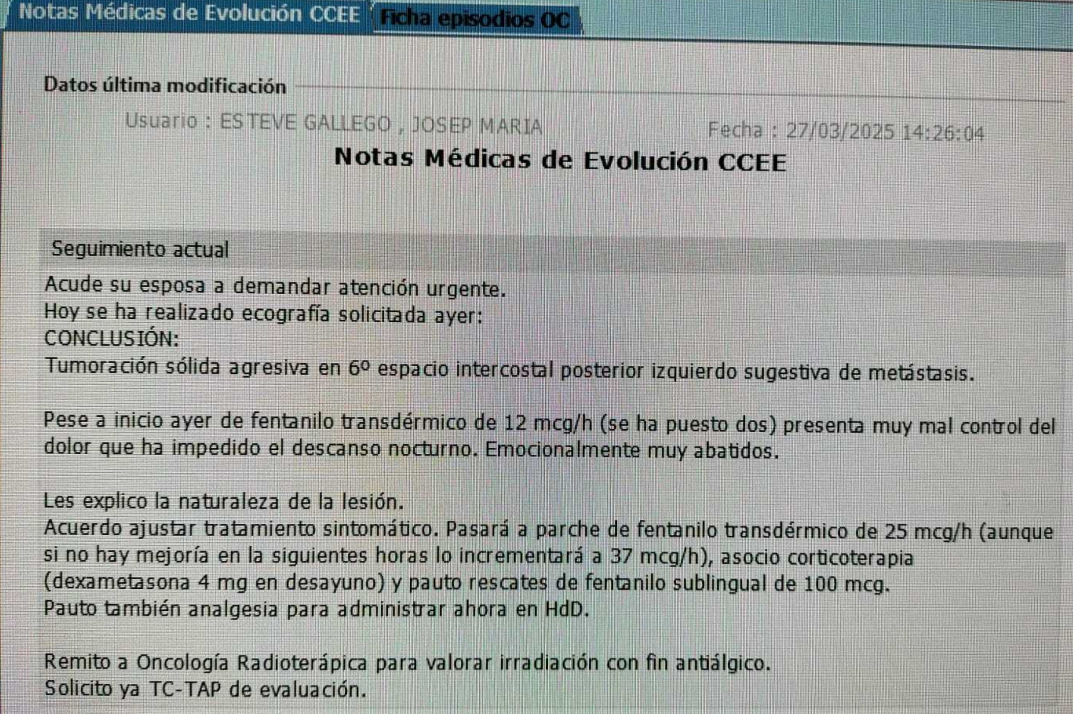
(03/29/2025) The back pain today is unbearable. I can't even sit in my office, which until now was one of the two places where I could be more or less without pain. I have to lie down, and even then it doesn’t go away. I take an Abstral (sublingual fentanyl) to try to control it.
On top of that, I have chills despite being well covered. I take my temperature around 1:00 p.m. and... fever! (38.7°C) I take a Paracetamol and wait an hour—same temperature. After more than two hours, the fever doesn’t go down, 38.8°C. Too high. In the end we had to call 112 and an ambulance took me to the ER at La Fe. I was admitted at 4:40 p.m.

Given my condition, I barely had to wait. They put me in an observation bed, with IV fluids, vital signs monitoring, etc. The goal was to see if there was some kind of infection, since chemo severely lowers your defenses. After full tests, they found nothing. They also did another chest X-ray, in case something showed up there. Nothing.
They’re giving me preventive antibiotics via IV, plus pills to take for a week. Pain management with Abstral, as needed, maximum 3 per day, plus the patches. If I needed more, I’d have to be hospitalized for pain control. Paracetamol for the fever; if it comes back, I’d have to return to the hospital.
At 3 a.m., I get home in an ambulance!
Shitty day.
(03/31/2025) Cold sensitivity in hands and feet is similar to last time. At least it hasn’t gotten worse. This time, while I was being administered Oxaliplatin, I followed a method called icing. Basically, it involves putting your hands in ice (ideally your feet too) and keeping ice in your mouth during that period. It’s somewhat painful and uncomfortable, because on top of being in contact with something so cold, you’re also more sensitive. However, since it doesn’t seem to have gotten worse this time, I might try it again next time.
I feel a bit tired and drowsy, which seems normal considering everything I’m taking.
 More intense cold sensitivity in the fingertips and mouth than the previous time. Now also in my toes.
Fatigue on the third day.
More intense cold sensitivity in the fingertips and mouth than the previous time. Now also in my toes.
Fatigue on the third day.
(16-03-2025) Pounding headache on the 5th day after starting.
It seems that the insomnia is subsiding. It's possible that it was caused by the corticosteroids, according to what I've been told. I'm in the process of stopping them.
 Cold sensitivity in the fingertips and mouth for 2 or 3 days. Fingers feel bloodless, and the tips hurt. Insomnia.
On March 4th, on the sixth day, I have a fever of 38 degrees that goes away 2 or 3 hours after taking a Paracetamol. I don't have a fever again.
Cold sensitivity in the fingertips and mouth for 2 or 3 days. Fingers feel bloodless, and the tips hurt. Insomnia.
On March 4th, on the sixth day, I have a fever of 38 degrees that goes away 2 or 3 hours after taking a Paracetamol. I don't have a fever again.
Insomnia.
 I spend 4 or 5 days completely drained of energy, with intense fatigue. Gradually, I start recovering. Insomnia.
I spend 4 or 5 days completely drained of energy, with intense fatigue. Gradually, I start recovering. Insomnia.
In my background, I do not have dyslipidemia (not having shown alterations in lipid levels at any given time), but I do have familial hypercholesterolemia (genetic predisposition to have elevated cholesterol levels, particularly LDL).
| Test | Normal ranges |
|---|---|
| Colesterol | 140 - 250 |
| LDL Colesterol | 80 - 180 |
| HDL Colesterol | 35 - 65 |
| Trigliceridos | 0 - 170 |
| Test | Normal range | Units |
|---|---|---|
| AST/GOT | < 40 | U/L |
| ALT/GPT | 10 - 45 | U/L |
| GGT | 7 - 70 | U/L |
| Alkaline phosphatase | 40 - 130 | U/L |
| Total bilirrubin | 0.3 -1.20 | mg/dL |
After a chemo session these values can be even three times higher and it's considered "normal". Above those, it needs to be assessed.
| Test | Normal values | Units |
|---|---|---|
| LEU Leucocitos totales | 3.50 - 10.50 | 10³/uL |
| NEU Neutrofilos | 1.9 - 7.3 | 10³/uL |
| LYM Linfocitos | 1.0 - 3.0 | 10³/uL |
| PLT Plaquetas | 150 - 400 | 10³/uL |